The medtech company of the future is an ecosystem enabler
The future of medtech: Orchestrating the next evolution of
Medtech is positioned at the intersection of diagnostics, devices, and data, uniquely equipped to design the infrastructure, standards, and governance that link technology to patient care. By leading this integration, the industry can evolve from an innovator of tools to an orchestrator of performance and outcomes across healthcare.
The tools of this transformation are already here. Robotics, intelligent sensors, and agentic AI are expected to fundamentally change how patient care is delivered and how caregivers are enabled. Interoperable platforms can enable information to flow securely and seamlessly across health systems, transforming both clinical and operational decision-making.
In hospitals, surgical robots integrate imaging and analytics to guide decisions in real time. In motion, connected wearables detect risks and prompt intervention before symptoms appear. At home, AI-enabled systems support daily care, guiding patients safely and independently under virtual oversight and targeted caregiver interventions. Together, these advances are set to redefine the boundaries of healthcare from centralized delivery to a distributed, intelligent network that learns with every interaction.
For medtech leaders, success hinges not just on innovation, but on integration and the ability to connect technologies, partners, and data into coherent systems that enhance outcomes, expand access, and strengthen the sustainability of healthcare.
Pressures shaping the future
The connected, intelligent, and accessible future we imagine won’t arrive automatically. Today’s healthcare system wasn’t built for it. Across the health industry, pressures are intensifying. Costs are rising faster than inflation, clinical capacity is stretched thin, data is multiplying faster than it can be used, and regulation is struggling to keep pace. These forces aren’t just challenges, they’re signals of where innovation is most urgently needed. For the medtech sector, they define the agenda for the next decade and where companies should focus, lead, and collaborate.
System strain—bending the curve on cost, capacity, and access
Healthcare is straining under the weight of its own complexity. Costs continue to rise faster than inflation, with annual growth approaching 8%.1 Hospitals are consolidating, and workforce shortages are intensifying. Some estimates suggest the U.S. could face a shortfall of nearly 200,000 physicians by 2037.2


At the same time, patients are struggling to access care. A third of consumers report delaying or skipping needed care due to affordability. These trends are unsustainable, both economically and socially.
Traditional, facility-based care models can no longer absorb growing demand. To bend the cost curve and expand capacity, healthcare should shift toward distributed, automated, and connected care.
This is where medtech has an opportunity to lead. By combining automation, robotics, and remote monitoring, medtech companies can help extend care beyond walls, amplifying the capacity of clinicians and empowering patients to manage more of their health from home.
Consumer expectation—the demand for convenience and personalization
At the same time, expectations of healthcare are changing. Consumers now bring the standards of digital life into their health decisions, seeking convenience, transparency, and personalization that traditional systems rarely provide. They want care that fits seamlessly into their routines, guided by insights that feel tailored to them.
This shift is expanding the definition of value. Medtech companies should now design not only for clinical efficacy but also for experience, creating technologies that are accessible, intuitive, and connected to the broader digital ecosystems people already use. Those that meet consumers where they are can drive adoption and trust across the care journey.
Data deluge—transforming insight into intelligent action
The healthcare system now generates more data than it can use. Each scan, lab, wearable, and device adds to the torrent, but integration remains limited. Valuable insights are trapped in silos, and clinicians often lack the tools to turn data into action.
Healthcare generates an estimated 30 percent of the world’s data, with a single hospital producing as much as 50 petabytes each year. Yet studies suggest that up to 97 percent of this data goes unused, and roughly 80 percent remains unstructured, limiting its value for clinical or operational decision-making.3 Evidence from interoperability and health-information-exchange initiatives shows that when data flows seamlessly, through standards such as FHIR (Fast Healthcare Interoperability Resources), organizations achieve measurable gains in care coordination, safety, and patient outcomes.
Next-generation devices and diagnostics will not only measure but interpret, communicate, and adapt. Interoperable systems, built on open standards and governed by trust, allow information to move securely across organizations, enabling real-time decisions that anticipate risk and personalize care. The future of medtech lies not in collecting more data but in connecting it.
Regulation refines boundaries and opportunities
As technology moves faster than policy, regulators should also rethink how innovation is evaluated and reimbursed. Public funding and value-based reimbursement models are changing what it means to be “innovative.” Success will depend on designing systems that generate measurable evidence of safety, outcomes, and value automatically and continuously.
Medtech’s role is not only to meet these expectations but to help shape them. By embedding evidence generation into design and supporting transparent standards for data and algorithmic performance, the industry can guide regulation toward enabling, instead of limiting, innovation.
Recent regulatory actions reflect this shift. In 2025, U.S. and European authorities introduced guidance that expands the use of real-world data and adaptive artificial intelligence across the medical device lifecycle, from post-market monitoring to iterative improvement. Together, these frameworks signal growing regulatory acceptance of continuous evidence generation, de-identified real-world data, and learning systems that evolve safely over time.
Ecosystems take shape: how the industry will evolve
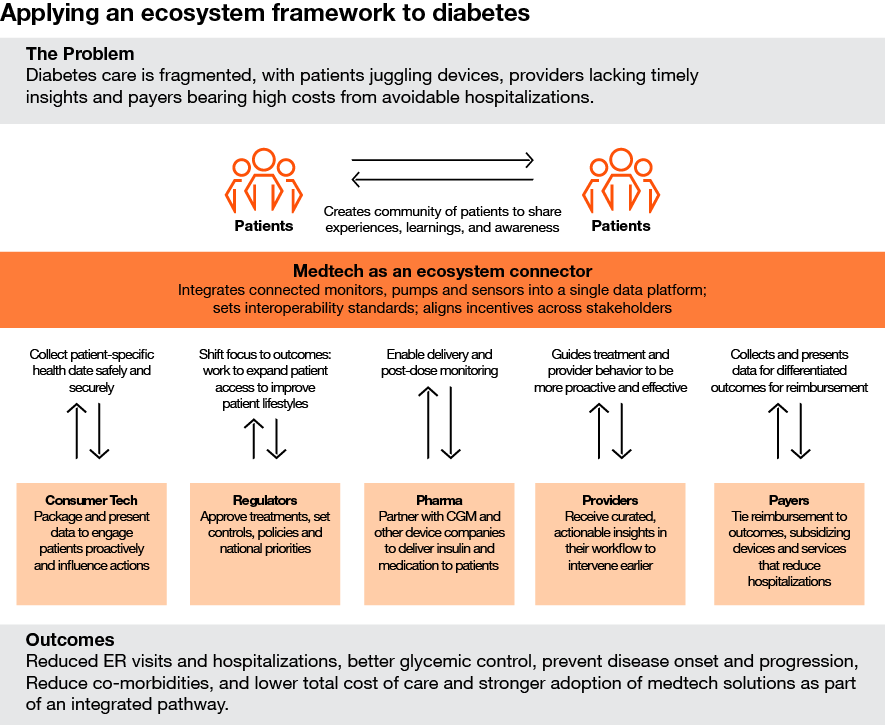
As system pressures converge, it’s clear that progress will depend on collaboration, not competition. The next decade’s breakthroughs will come from ecosystems, or networks of organizations aligning their strengths to solve challenges too complex for any one player.
These ecosystems unite medtech companies, providers, payers, pharmaceutical firms, technology companies, and others around shared outcomes. Each contributes a different capability, whether devices, data, analytics, or services, into a connected framework that improves efficiency, access, and results.
When they work well, ecosystems create continuous feedback loops that refine performance, align incentives, and build trust. Everyone benefits when information flows securely, outcomes improve, and costs decline.
For medtech, this marks a shift from selling products to enabling systems. Positioned at the intersection of diagnostics, devices, and data, medtech is uniquely equipped to design the infrastructure, standards, and governance that link technology to patient care. By leading this integration, the industry can evolve from innovator of tools to orchestrator of performance and outcomes across healthcare.
Growth vectors: Where ecosystems unlock value
The next era of growth will come from building connected ecosystems that integrate data, technology, and human expertise from hospital to home, spanning the entire journey of care. These three scenarios illustrate how medtech companies can shape ecosystems that will evolve to deliver value across settings of care.
1. Medtech in the hospital: From complexity to coherence
Inside the hospital, medical technology has become indispensable – from patient monitoring to surgical robotics and imaging to logistics. But ubiquity comes at a cost. Thousands of interconnected devices and data streams now operate side by side, often without a common language or organizing framework. What was once an advantage in precision is becoming a challenge in coordination.
The hospital of the future will require a new operating model, one that treats technology as a living infrastructure of intelligence instead of a collection of tools. In this environment, medical technology serves as the central nervous system of care delivery, translating information into insight and orchestrating action across people, processes, and places.
Ecosystem dynamics
Embedded sensing: Devices, surfaces, and supplies capture continuous streams of clinical and operational data that feed a shared intelligence layer.
Ambient AI: Context-aware algorithms interpret that data in real time to anticipate patient needs, predict deterioration, and automate routine documentation or administrative tasks.
Integrated robotics: Surgical and procedural systems connect seamlessly with imaging, navigation, and workflow platforms, enhancing precision, reducing variability, and improving recovery times.
Connected workflows: Interoperable communication systems unify clinicians, data, and equipment, transforming fragmented hospital operations into a synchronized network.
A connected, intelligent infrastructure can amplify human capacity by automating the repetitive, augmenting the complex, and enabling clinicians to focus their expertise where it is needed most. Predictive tools can help manage patient flow, reduce complications, and shorten length of stay, while real-time analytics improve asset utilization and throughput.
In this model, the hospital becomes an ecosystem of systems that are interoperable, data-driven, and continuously learning. Its performance improves with every interaction, building resilience against systemic pressures on workforce, access, and cost.
Medtech’s position in the hospital has always been one of partnership and precision, helping clinicians deliver safer, smarter care. Building on that legacy, the next opportunity is to connect these proven strengths to the wider health ecosystem. Success will depend on shared governance, open standards, and ethical frameworks that ensure automation enhances rather than replaces human judgment. For medtech leaders, this means evolving from supplying devices to linking what already works inside the hospital to the systems that extend care beyond it.
2. Medtech in motion: Connecting care in real time
As care moves beyond the hospital, medical technology is becoming continuous, mobile, and deeply interconnected. Devices that once existed in isolation now travel with the patient and are embedded in wearables, implants, and digital platforms that capture health data in real time. This evolution marks the rise of medtech in motion, an ecosystem that extends clinical intelligence into everyday life.
In this environment, the line between medical technology and digital health blurs. Every measurement, whether monitoring a joint replacement, a glucose level, or cardiac rhythm feeds a shared data infrastructure that links patients, clinicians, and systems in real time. Information no longer stops at the point of care. It moves with the individual, transforming how we understand health, risk, and recovery. Connectivity is only the starting point. The real advantage lies in the ability to turn shared data into shared intelligence, aligning decisions and actions across the ecosystem.
Across medtech, connected technologies are already showing how data, intelligence, and collaboration transform standalone devices into coordinated systems of care:
Remote patient monitoring for chronic disease:
AI-enabled cardiac and pulmonary monitoring programs are reducing hospital readmissions for heart failure and COPD by detecting deterioration early and triggering proactive virtual interventions.
Neuro and brain–computer interfaces:
Next-generation BCI and neuromodulation platforms convert brain or nerve activity into digital signals that guide continuous monitoring, adaptive therapy, and personalized rehabilitation.
Digitally enabled orthopedic solutions:
Connected implants and wearable sensors capture movement and recovery data, linking patients, clinicians, and care teams to track outcomes and optimize rehabilitation in real time.
Integrated metabolic and lifestyle monitoring:
Cross-category integrations are connecting continuous glucose, sleep, and activity data to create comprehensive health profiles—enabling both clinical oversight and patient self-management.
Ecosystem dynamics
Real-world evidence: Continuous data from connected devices becomes the foundation of modern evidence generation, capturing safety, efficacy, and performance in real-world settings.
Integrated health networks: Data from multiple domains: orthopedics, cardiology, metabolic health, pain management and others, converges to create unified patient profiles and cross-specialty insights.
Adaptive learning loops: Device performance and outcomes feed directly back into design, therapy guidance, and payer models, creating a self-improving system that learns at scale.
Collaborative infrastructure: Medtech, healthtech, and payer partnerships enable secure data exchange, interoperability, and shared analytics that extend the value of every connected product.
Through this mobility, care becomes continuous and anticipatory. Predictive analytics can identify risk earlier, guide intervention, and personalize therapy reducing readmissions and improving outcomes across populations. For clinicians, it closes the gap between episodic visits and lived experience. For systems, it enables performance-based care and faster learning cycles. For patients, it transforms monitoring into empowerment.
In this model, medtech serves as the connective tissue of a distributed health ecosystem, linking people, data, and outcomes in motion. Leadership in this space will depend on designing for interoperability, trust, and continuous learning to build ecosystems that move with the patient and evolve with every data point.
3. Medtech at home: Extending the ecosystem to everyday life
The home is rapidly emerging as a vital part of the health ecosystem. Advances in robotics, remote monitoring, and AI-guided care are transforming living spaces into micro-clinical environments capable of monitoring, diagnosing, and even treating conditions once confined to hospitals. This evolution signals a fundamental shift from health systems organized around facilities to ecosystems organized around people.
In this new paradigm, care follows the individual. Devices, data, and digital platforms work together to support continuous engagement between patients, clinicians, and caregivers. The home becomes not an endpoint of care, but a fully integrated extension of the clinical network – connected, intelligent, and adaptive.
Ecosystem dynamics
Augmented human care: Assistive robotics and automation extend the reach of clinicians and caregivers, supporting mobility, rehabilitation, and daily living while preserving the human connection at the heart of care.
AI-enabled self-management: Intelligent systems help patients monitor conditions, adjust treatments, and access guidance under virtual physician oversight.
Last-mile integration: Partnerships across retail, logistics, and pharmacy networks bring diagnostics, therapeutics, and connected devices directly to patients, ensuring timely access and continuity of care.
Trusted connectivity: Secure data infrastructure links home-based systems with providers and payers, maintaining data integrity and privacy while enabling proactive, coordinated interventions.
In this model, the boundaries between clinical and personal spaces dissolve. Continuous feedback from home-based technologies enables earlier detection, more precise management of chronic conditions, and reduced dependence on hospital capacity. The result is a system that brings high-quality care to people rather than bringing people to care.
For medtech leaders, this evolution requires a shift in mindset, from building devices for controlled environments to designing ecosystems that thrive in the variability of daily life. Success will depend on understanding human behavior, embedding trust and usability into every interaction, and collaborating across sectors to make connected care effortless and equitable.
Imperatives for medtech leaders: What you should do now
Building these systems, across the hospital, in motion, and at home, will demand clarity of purpose and precision of partnership. Companies must identify the problems they will take on, who should be at the table, and how to translate intelligence into measurable value. The next generation of medtech leaders will not compete on ownership, but on orchestration and their ability to design systems that learn, adapt, and create shared value across the entire continuum of care.
1. Define your ecosystem.
Start with a problem worth solving. Focus on specific health or system challenges and build partnerships around that goal. For example, improving outcomes across care pathways in cardiovascular or orthopedic procedures, enabling earlier intervention for patients managing chronic disease outside the hospital, or improving operational efficiency through connected workflows.
2. Identify your partners.
Determine who should be at the table: payers, providers, technology platforms, regulators, and patient organizations. Clarify what each brings: data, distribution, trust, capital, and align on shared incentives.
3. Clarify your role.
Not every company will lead. Some will act as connectors, setting standards and governance; others as activators, investing heavily to scale; others as participants, bringing specialized capabilities. The key is to know your role and commit to it.
4. Build for outcomes.
Design products, data systems, and services that deliver measurable value including lower complications, reduced cost, and improved experience. Treat outcomes as the central product, not an afterthought.
5. Rewire your operating model.
Integrate AI and data across every function: R&D, supply chain, quality, commercial. Build capabilities for continuous learning, evidence generation, and rapid iteration. The companies that treat data as a living asset will adapt fastest to changing markets and regulations.
The moment to lead
The next decade will determine which medtech companies evolve and which fade into the background. The winners will be those that move first to connect technologies, data, and partners into ecosystems that improve outcomes, expand access, and create a more resilient healthcare system.
For decades, medtech has driven innovation inside hospitals. Its next great contribution will be enabling a more predictive, more connected, and more human system that works better everywhere. This transformation won’t come from technology alone but on leadership, trust, and collaboration across sectors.
The direction is clear: The future of medtech is about building the infrastructure of intelligent, coordinated care and companies that act now will define how health is delivered for a generation to come.
The future of healthcare
Over the next decade, we expect $1 trillion of annual healthcare spending to shift.
Next in medtech 2025
The next 12–24 months are a critical window for medtech.















