{{item.title}}
{{item.text}}

{{item.text}}
Our solution can help prevent patient leakage by managing both provider time and the moments that matter most in a patient’s care. This can include preventive insights, provider capacity recommendations and front door transformation. Combining these capabilities with a technology solution can enable proactive management and better patient-to-provider matches based on preferences and known clinical data.
Salesforce can be leveraged in a technology-enabled solution to identify and resolve these problems.
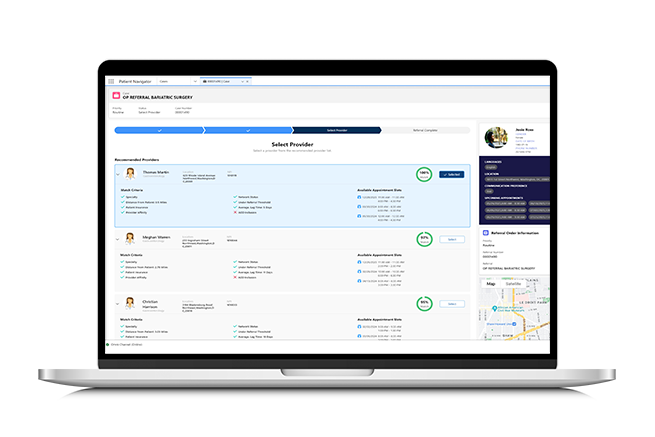
Our proprietary technology can: 1) identify optimal provider matches based on important factors such as appointment availability, geographic proximity, network affiliation, and patient preferences; 2) streamline referral processes with the enhanced user interface, designed to facilitate effective and prioritized referral management and 3) empower your organization with data-driven decisions and superior patient care coordination, helping you to enable a new standard in healthcare excellence.
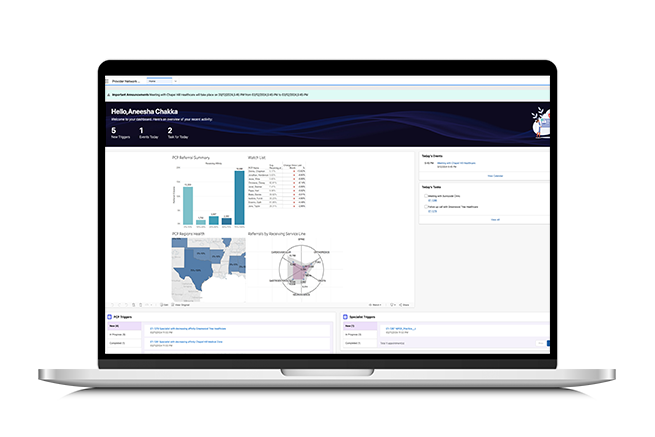
Leverage our advanced PCP and Specialist dashboards to gain valuable insights into provider referral behaviors. View key performance indicators (KPIs) for referrals, which can be segmented by providers, service lines, and affinities. This powerful tool can help healthcare leadership make informed decisions, improve referral patterns and enhance overall service delivery.
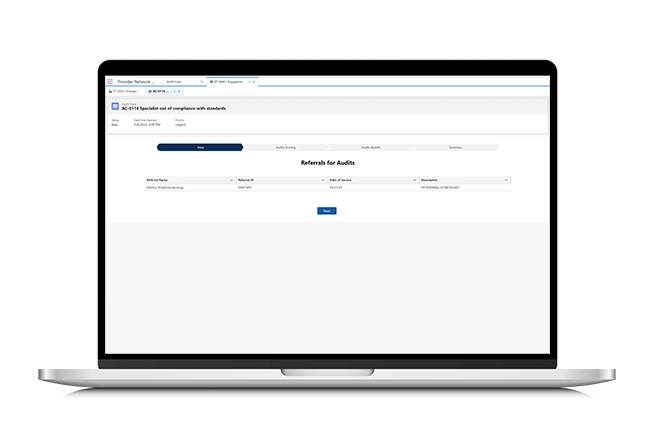
Programmable alerts set to specific engagement triggers help indicate divergences in provider referral behaviors and are used to track progress. Built-in processes and tools help evaluate engagement triggers and initiate service line audits. The Individualized Provider Dashboard can provide easy access to provider referral history for investigation.
{{item.text}}

{{item.text}}