healthcare reboot for the gcc
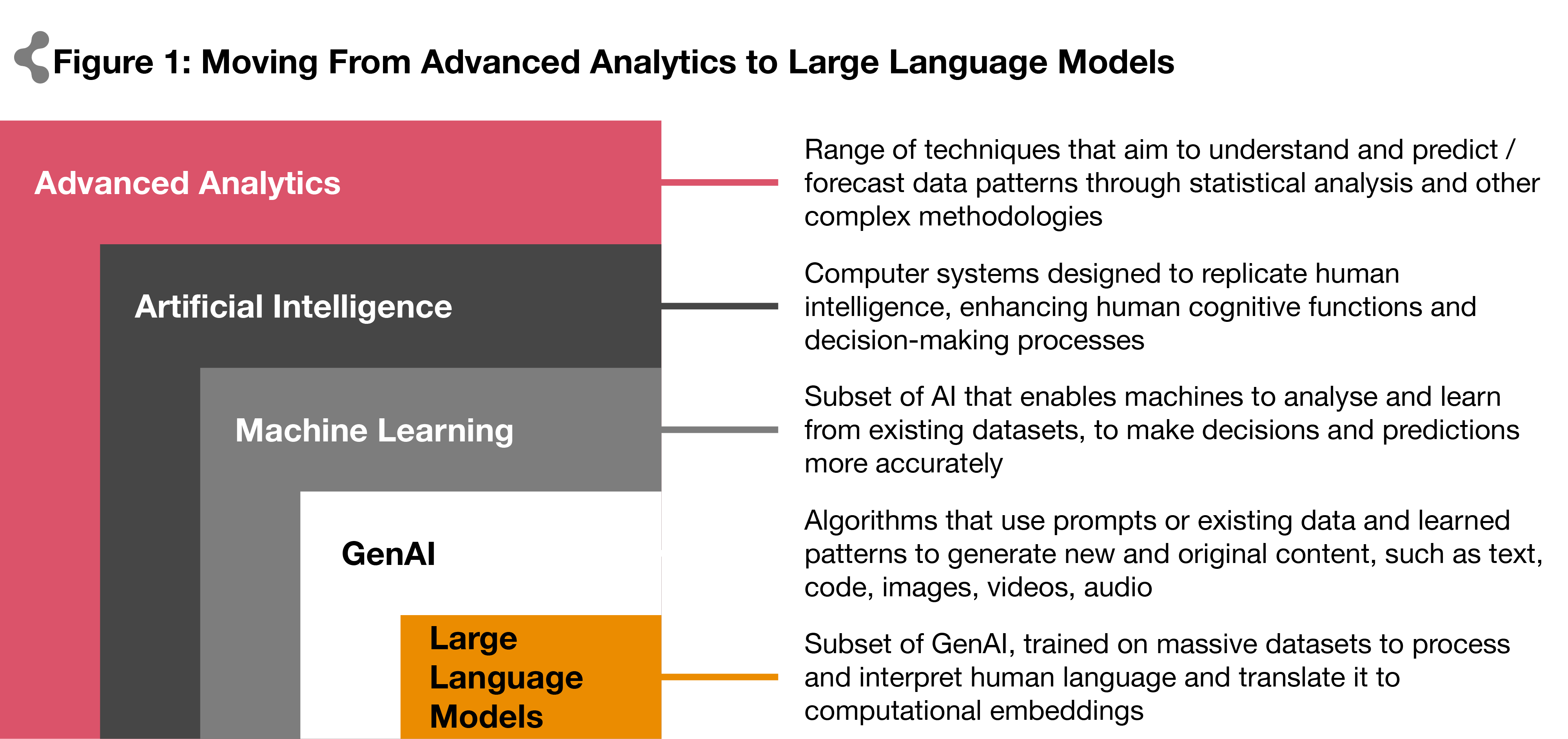
Artificial Intelligence (AI) in healthcare is no longer a distant dream. Natural language processing (NLP) can, among other things, now record doctors' notes, interpret medical histories, and analyse scientific literature more thoroughly than humans. Deep-learning algorithms applied to wearable sensors, genomic data, blood work, scans, and other medical information can develop personalised treatment plans. And virtual medical assistants powered by AI can offer health coaching, shape diets, and even help prevent and predict illness.
AI in healthcare analytics has evolved from basic data patterns to complex predictive models. Leading institutions use AI to analyse vast amounts of clinical data, improving diagnosis and workflows. Mayo Clinic's virtual primary care system in the United States, for example, uses AI to optimise patient interviews and diagnostic processes, with physicians selecting AI-recommended diagnoses in 84% of cases.
In 2008, the Singapore Ministry of Health established Synapxe (originally the Integrated Health Information System) to connect people and systems for a healthier Singapore. Partnering with major technology providers, Synapxe developed the AI-powered Health Discovery Plus (HD+) system, enhancing healthcare services and workflows. HD+ supports remote monitoring and management of conditions like hypertension and chronic kidney disease. Developed during the pandemic, it significantly improved patient care by processing over 660,000 vital sign reports and issuing over 45,000 clinical alerts. Innovations like HD+ demonstrate AI's potential in remote patient monitoring, diagnostics, and patient-managed treatment planning, driving global healthcare toward AI-augmented care.
Although interest in healthcare AI opportunities has been growing exponentially over the past few years, its roots began in some of healthcare’s greatest challenges. For the past five decades, healthcare technology has been plagued by a lack of interoperability - getting data and people to communicate intelligently, quickly, and efficiently.
The more recent emergence of Generative AI (GenAI) addresses a major challenge in healthcare: the overwhelming amount of unstructured data from diverse sources. It does this by extracting insights from complex datasets, such as millions of whole genome sequences or human brain intricacies. As leading physician Eric Topol explains in his published work, Deep Medicine, these advancements will ultimately enhance the health outcomes for individuals and improve the efficiency of healthcare providers.
GenAI also supports clinical documentation and patient interactions by automating tasks such as transcribing clinical notes and managing insurance claims. AI-powered virtual assistants enhance the patient experience by handling inquiries, scheduling appointments, and authorising insurance, providing personalised and efficient service without additional costs.

(2,3)
Recent examples of AI healthcare initiatives in the region:
The UAE has been making great strides in leveraging AI in healthcare - from Abu Dhabi’s Department of Health becoming the first entity to develop the Policy on Use of Artificial Intelligence in the Healthcare Sector9, through to the Ministry of Health and Prevention (MoHAP) establishing the health sector’s inaugural Centre of Excellence for AI in 202310. Earlier this year, Thumbay Institute of AI in Healthcare hosted the regions first international conference on AI training and upskilling for healthcare professionals11.
The Dubai Health Authority’s EJADA AI system has also achieved remarkable results through a preemptive disease prevention system, while the UAE healthcare firm M42, a joint venture between Mubadala Health and G42 Healthcare, has recently launched Med42, a clinical Large Language Model that provides high-quality answers to medical questions. This follows the earlier release of their Arabic-enabled 'Jais' model, showcasing the country’s commitment to advancing healthcare through AI.
Recently in Saudi, the Saudi Data and AI Authority established the AI Ethics Principles to integrate AI technologies, regulate AI data, safeguard data privacy, promote responsible AI development, and minimise risk12. And in 2022 the Saudi Food and Drug Authority published guidance on the regulation of AI and ML-based medical devices, to ensure the safety and reliability of these technologies13.
With governments laying the groundwork for AI governance, healthcare entities now have an urgent responsibility to integrate these technologies within their businesses, to make sure they are on track with the global mobilisation as they strive to meet enterprise challenges.
Stabilisation, value-based care, and regulation drive AI direction across the GCC
In the current environment, healthcare demand is largely well-served by high-quality, specialised providers, and market expansion is tapering as it approaches a steady state. As business value growth potential levels off for healthcare providers across the GCC, the focus for players is reorienting towards differentiation and improving efficiencies.
Stabilisation is also inevitable with the various government reforms in place aimed at expanding private health insurance coverage. Abu Dhabi and Dubai have witnessed this with the rollout of mandatory insurance, resulting in steady hospitalisation rates of around 10% following full implementation14. Other GCC countries are expected to follow a similar trend.
With the increased focus on value-based care — succinctly defined as the overall cost of improving outcomes that are valued by patients and populations—the overarching message is evident: providers are incentivised for the value of integrated care they provide. In Abu Dhabi, downward pressure on facility multipliers has been witnessed from a reimbursement standpoint, thus impacting overall business top line growth. Similar to the case in Dubai, the potential introduction of service-based packages in the region is also expected to exert negative pressure on expected reimbursement rates. Providers are thus forced to deliver care more effectively by leveraging operational efficiencies—an approach that can be facilitated through the use of AI. By applying AI algorithms, processes such as resource allocation, including staff scheduling, room utilisation, and equipment maintenance, can be streamlined, thus improving overall efficiency.
Growing regulatory requirements and maturing insurance markets have also increased the imperative for physicians and other clinicians to accurately document patient information, thereby increasing the administrative burden and limiting the time they have available to fulfil their true purpose: treating patients face to face. This is amplified by the shortage of clinical staff in the GCC and the heavy reliance on external staff to fill the resource gap, with recent findings showing close to 60% of physicians and nurses in KSA and Oman being expatriates (this figure rises to more than 90% in Dubai alone, highlighting how expat-driven the workforce is)15. To mitigate this issue, GenAI offers the solution for auto-generating necessary clinical documentation and relieving the administrative burden.
Given the challenge presented by governments moving forward with AI governance and the market pressures in the region, how does the healthcare sector move forward with exploiting the opportunities inherent in AI technology? As with many disruptive technology adoptions, it begins by making the business case.
The GCC— a region ripe for AI-enabled technological innovation
GCC governments are aligning with the global digital revolution, shifting their focus to e-commerce, smart cities, e-services, and digital health. These indicators and growing enthusiasm have paved the way for AI to be integrated within businesses from all sectors, including a leapfrog adoption cycle for AI across the healthcare sector.
To realise the full potential of AI, societies and organisations must commit to advanced healthcare analytics. This commitment is already underway in the Gulf Cooperation Council (GCC) region. In fact, our research highlights the GenAI market opportunity across the GCC, estimating potential overall economic impact of $23.5 billion per year by 2030. The research also indicated that GenAI-fueled improvements in efficiency and effectiveness would have the greatest impact in Saudi Arabia and the UAE, with significant benefits also seen in Qatar, Kuwait, Oman, and Bahrain and healthcare was one of the key industries to be affected, along with media and entertainment, banking and financial services, and IT and telecommunications.
GCC AI readiness indicators
(4,5,6,7,8)
Getting started in healthcare AI implementation
Implementing an AI programme can be an exciting yet daunting endeavour for leadership teams looking to harness its transformative power. In healthcare today, AI offers unprecedented opportunities to drive innovation, enhance decision-making and unlock new levels of efficiency and competitive advantage.
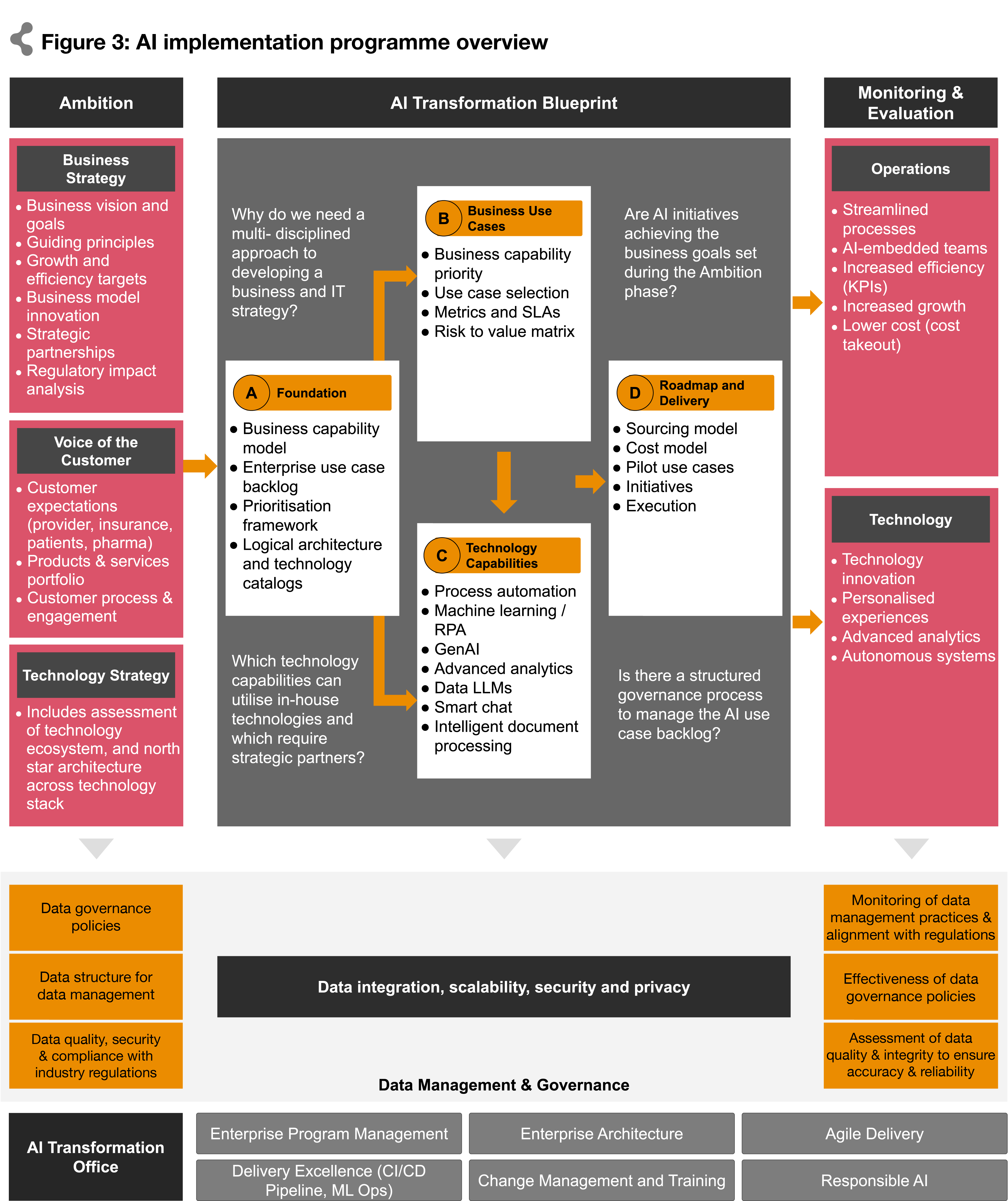
By structuring AI work into three phases, leadership can establish a clear plan from strategy through execution and measurement. This structured approach aligns teams and maximises AI’s impact on business operations, customer experiences and technology innovation. To drive this process, an AI Centre of Excellence (CoE) can be established, which will serve as a stepping stone to capture, ideate and develop use cases, and build internal capacity in a responsible and sustainable way.
15
Phase 1: Ambition
Leadership starts by identifying appropriate business and technology team members. The Ambition phase sets the overarching business, technology, and data strategy for the AI programme, taking an outside-in, customer/product-centric approach. Key activities include defining AI vision and goals, aligning customer needs and market trends, and establishing clear success criteria for measuring AI’s impact on customer experiences. This phase assesses the readiness and investment requirements for AI adoption, and establishes governance structures and stakeholder engagement mechanisms to ensure alignment and accountability throughout the AI journey.
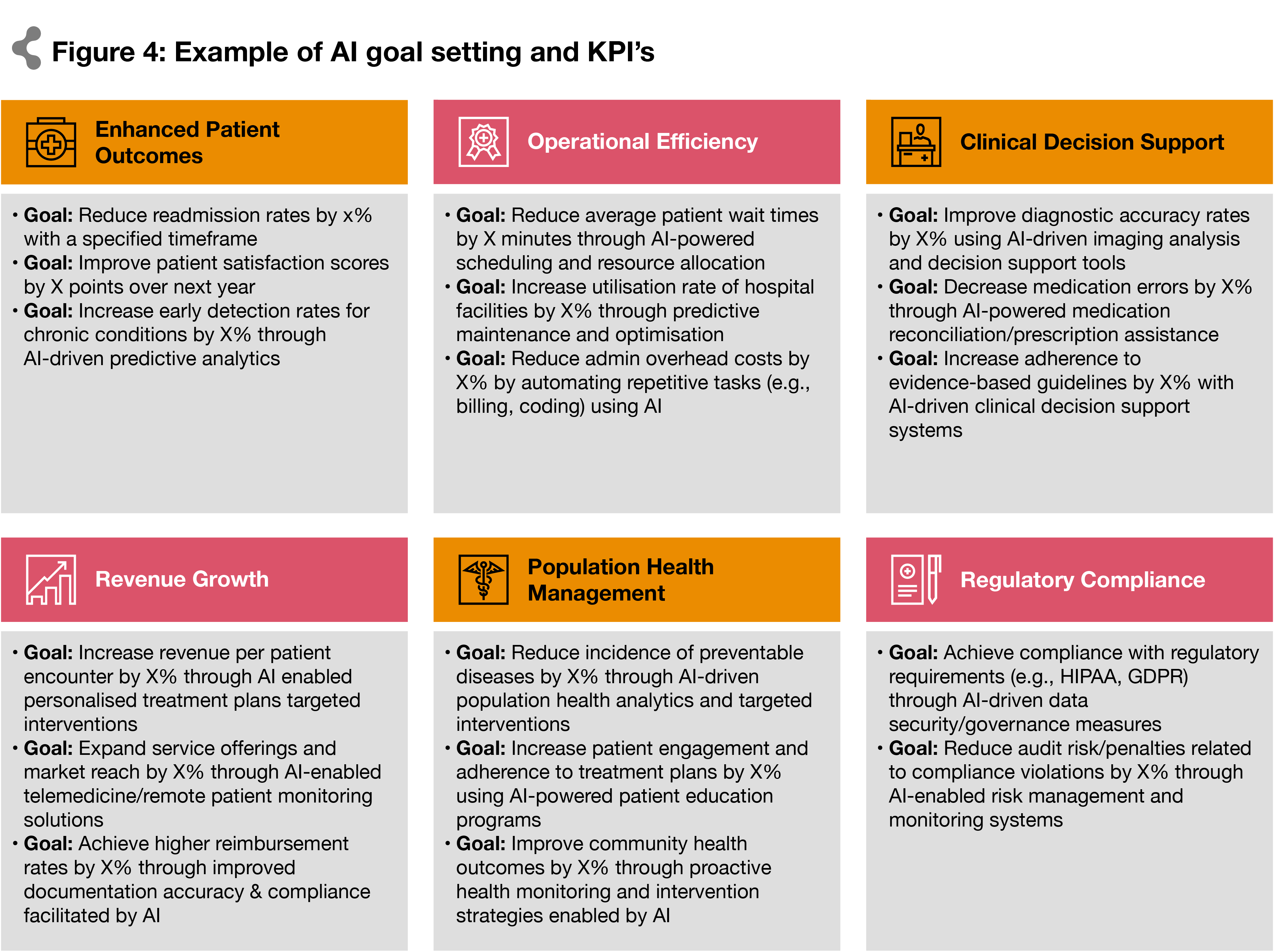
Leadership teams should define quantifiable business goals using key performance indicators (KPIs) to demonstrate AI’s impact, ranging from improving patient outcomes and operational efficiency to driving revenue growth and ensuring regulatory compliance. By setting clear, measurable objectives, leadership can track progress, evaluate efficacy, and demonstrate tangible value to stakeholders.
also important to thoroughly assess what data is available, including the different sources, formats and quality of the data that will need to be leveraged. Identify any gaps or concerns that might exist, and develop a plan to source, prepare and integrate the data required in a robust and responsible way.
Phase 2: AI Transformation Blueprint
The AI Transformation Blueprint phase builds a roadmap that balances value and risk, and flows from the business strategy and KPIs of the Ambition phase into developing AI business use cases and priorities for engaging AI technology capabilities. Leadership assesses where the greatest opportunities lie for optimising existing processes within their current workflows. Leaders may also choose to prioritise certain initiatives based on unique needs and priorities, such as customer expectations or specific products and services in the enterprise’s portfolio.
Potential business use cases
The figure below illustrates a selection of potential business use cases for AI in healthcare, highlighting a spectrum of applications. We have identified and catalogued over 1,000 such use cases, demonstrating the extensive opportunities AI presents across various aspects of the sector:
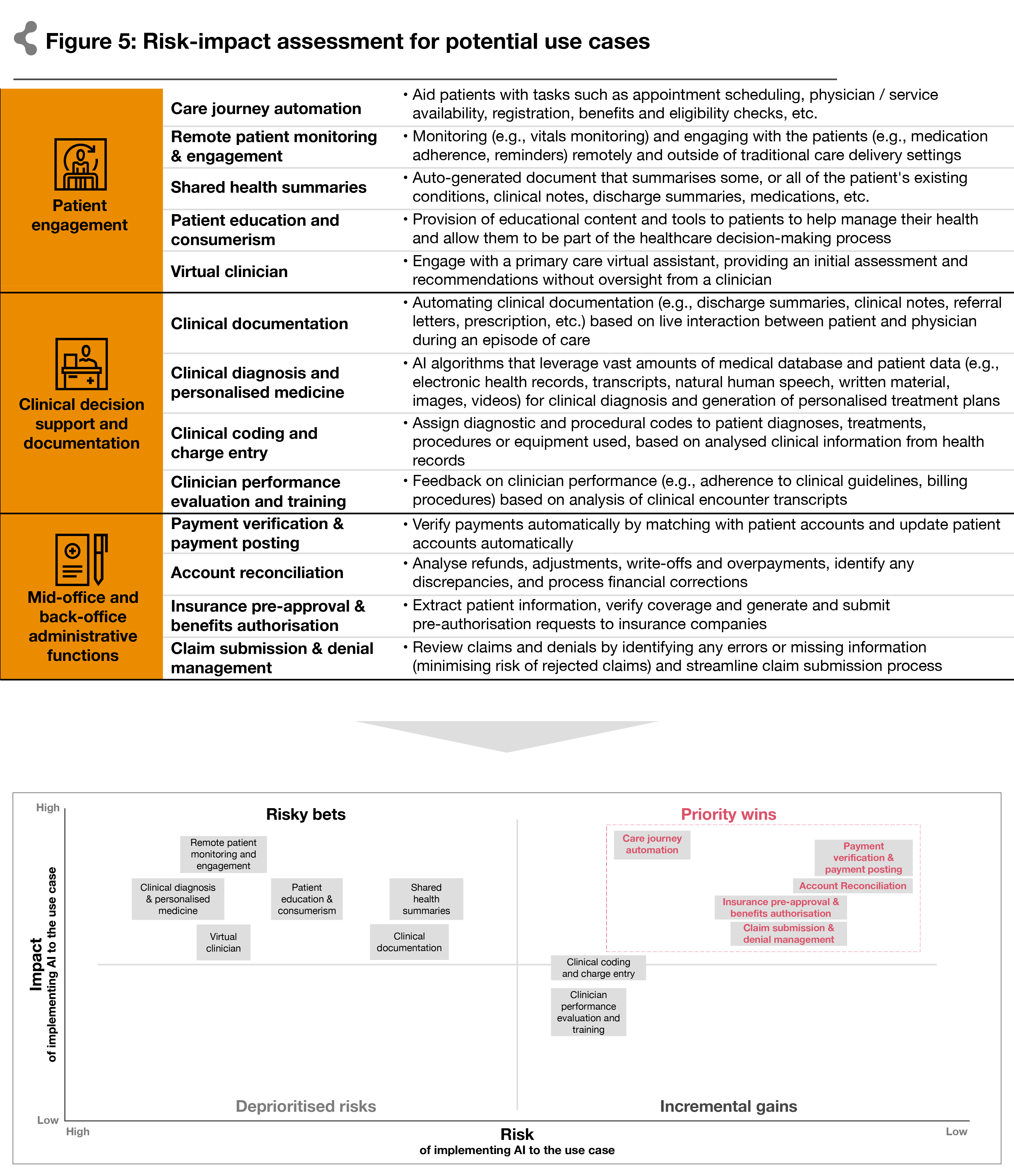
In developing and prioritising business use cases, leaders must define them in detail, including their objectives, target user groups, data requirements, and expected outcomes. Enabling technology needs are concurrently assessed, and a technology stack is selected or developed to effectively support AI use cases. The rapid advancement of AI technologies can lead to significant changes in risk and feasibility within a few months, necessitating continuous reassessment to ensure alignment with the latest developments and opportunities.
Partnership strategies
Partnership strategies also play a key to this analysis, covering both technological capability and the regulatory sides. Technology partners can provide access to cutting-edge, off-the-shelf AI solutions and domain-specific accelerators. Partnering with regulatory bodies and standards organisations can help mitigate legal and ethical risks associated with AI implementation.
Workforce and skills
A thorough review of the existing workforce skill sets must take place to identify any gaps where upskilling is required, or new roles to be created calling for fresh skills and experience entirely. Our latest CEO Survey found that 67% of Healthcare CEO's believe that GenAI will require most of their workforce to develop new skills. Workforce preparation is essential to successful execution.
Risk assessment
Leadership should also assess the potential for unintended consequences or disruptions to existing workflows and revenue cycle operations. By conducting a thorough risk assessment and weighing these factors, business leaders can make informed decisions about which processes to prioritise for AI initiatives and mitigate risks effectively. Risk also has to be measured against value to determine priority. High-risk factors, such as external versus internal customers (i.e. patient facing vs. employee facing), regulatory compliance, data security, and stakeholder buy-in, must be carefully evaluated to mitigate potential challenges and ensure successful implementation.
Once potential use case areas have been identified, leaders can evaluate which elements can be served using in-house technology capabilities versus which will require strategic partnerships. At this point teams can also collaborate to define clear objectives, success criteria, and KPIs for each use case.
By following a structured approach to use case development, leadership teams can ensure that AI initiatives are aligned with strategic objectives and positioned for success in driving tangible business value and innovation. This phase also involves building or enhancing data infrastructure, sourcing and preparing training data, and developing or acquiring AI models and algorithms. Finally, the AI Transformation phase outlines a comprehensive implementation plan, including timelines, resource allocation, risk management strategies, and milestones for measuring progress and achieving key deliverables.
For payers and pharma players, a similar approach can be adopted — prioritising individual use cases based on their value addition as well as their risk of implementation. Rather than having customer centres answering benefits-related questions, AI can automatically generate Explanation of Benefits tables that outline services and cost-sharing amounts, streamlining the workflow and reducing admin work. Payers can also facilitate prior authorisation processes through automated intake, validation and triaging of PA request documentation. This will help reduce waiting times for approvals, allowing patients quicker access to necessary treatments. Also, given the significant number of grievances and complaints insurers receive, automating the response process can expedite the workflow, as well as help in highlighting potential risks to minimise litigation and maintain brand reputation.
Pharma players can also leverage AI across different processes. By predicting and visualising molecular conformations, new molecule generation is enabled with data-informed models. AI can also enhance search and analytics capabilities through pretrained LLMs on available drug safety data and real-world cases. Additionally, companies can enhance manufacturing efficiency and compliance by automating electronic batch record (EBR) mining. This includes data collection and analysis, ensuring EBRs are compliant with regulations, and identifying deviations in manufacturing for quality control purposes.
Phase 3: Monitoring and Evaluation
The Ongoing Evaluation phase focuses on evaluating the outcomes of AI initiatives and measuring their impact against the overarching strategy. This involves defining KPIs and metrics to assess the effectiveness, efficiency, and ROI of AI programmes. These metrics may include customer satisfaction scores, revenue growth, cost savings, operational efficiency gains, and other relevant indicators. This also includes conducting regular assessments to track progress, identify improvement areas, and adjust strategies and tactics as needed. Additionally, this phase aims to communicate results and insights to key stakeholders, including senior leadership, business units, and external partners to recognise successes, address challenges, and reinforce the value of AI in transforming customer experiences and driving business outcomes.
With great power comes great responsibility: building an enterprise governance framework for responsible AI
For business leaders, there are plenty of reasons to be excited about AI, starting with its power and ease of use. But, as with any emerging technology, there are also potential new risks. Some of these hazards may come from your company’s use, others from malicious actors.
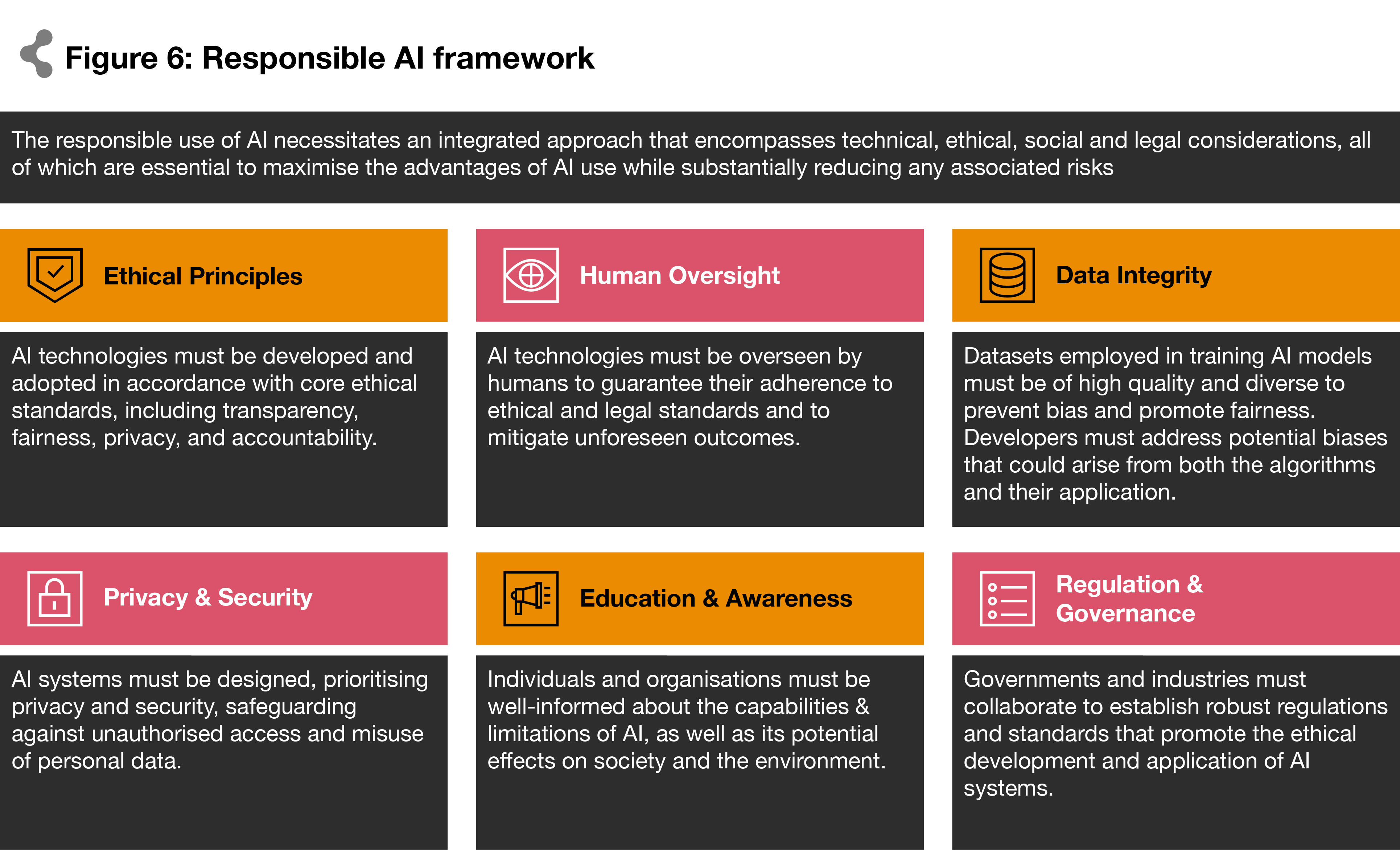
To manage both kinds of risks and harness AI’s power to drive sustained outcomes and build trust, you will need responsible AI - a methodology designed to enable AI’s trusted, ethical use. It has always been important, but it has become crucial in the dawning era of generative AI.
Healthcare leaders will start with a responsible AI end-to-end enterprise governance framework which focuses on the risks and controls that will guide the AI journey. The elements of such a framework are shown below:
What’s next?
AI is no longer a technology of the future: it is very much here and in use today. It holds the promise of empowering healthcare leaders to overcome some of the sector’s most historically daunting challenges—detecting diseases at their earliest stages, streamlining patient care, reducing medical errors, decreasing clinician burnout, lowering system costs, and improving outcomes that matter to the populations it serves.
It is not a question of whether healthcare will implement AI, but of how the implementation will proceed and continue to evolve. This raises a host of other questions for healthcare players in the GCC:
Where should healthcare players place their bets?
What should these entities focus on moving forward?
Should players take immediate action and invest in high-cost technologies, following global counterparts and best practices, even if they may pose some form of risk?
Or should players progress in small steps focused on low risk and low cost solutions (quick wins) to check the box for AI integration?
Do organisations have the minimum level of data quality, completeness, and maturity to enable the use of AI?
How will healthcare providers gain the trust of patients in clinical diagnosis and data privacy?
- How smoothly can they transform existing healthcare systems and workflows into digitised, AI-enabled processes?
The answers lie in a structured approach like the one we have detailed, driven by establishing a robust AI CoE from strategy to execution that can prioritise the right use cases while empowering the workforce with necessary skills and tools to augment their knowledge and capabilities.
The faster leadership teams can embrace AI and start their journey, the faster they can reap the many advancements that are driving costs down while improving quality of care. Achieving the delicate balance between innovation and risk mitigation is key to unlocking the full potential of this powerful and transformative technology
AI stands poised to reimagine healthcare. Where will your imagination lead your enterprise?









